Preparing Osteoporosis Patients for Dental Implant Procedures
all-on-x.online
November 19, 2024

Understanding Osteoporosis and Its Impact on Dental Health
Osteoporosis is a medical condition characterized by a decrease in bone density and quality, leading to an increased fragility of bones and a higher risk of fractures. This systemic condition predominantly affects the skeletal system, making bones more porous and susceptible to injuries. While osteoporosis is commonly associated with fragile hips, wrists, and vertebrae, its impact extends beyond these areas, significantly influencing dental health as well.
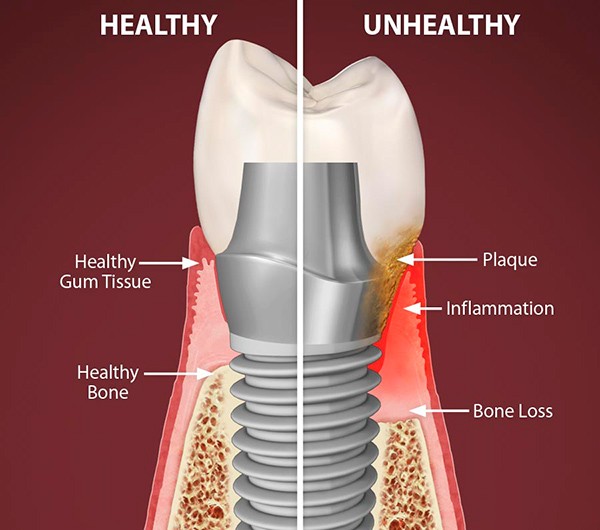
The role of bone density in dental health is paramount, especially concerning the jawbone. The alveolar bone, which supports the teeth, can lose density in individuals with osteoporosis, resulting in diminished structural integrity. This loss can pose challenges for dental implant procedures, as adequate bone density is crucial for the successful integration of implants. Insufficient jawbone density may lead to complications such as implant failure, increased healing time, and aesthetic concerns.
Moreover, understanding the relationship between osteoporosis and dental health is essential when planning any dental procedures. Patients with osteoporosis may experience a prolonged healing process, as their body’s ability to regenerate and repair bone tissue is impaired. This situation necessitates careful evaluation and consideration by dental professionals to ensure optimal outcomes. Techniques such as bone grafting or the use of implants designed specifically for low-density bone may be necessary in such cases, highlighting the importance of personalized treatment planning.
Ultimately, recognizing how osteoporosis affects both bone structure and dental health is crucial for healthcare providers and patients alike. Addressing the complexities of this condition will not only improve the outcomes of dental interventions but also enhance the overall quality of care for individuals living with osteoporosis. A proactive approach is essential for ensuring the successful management of dental health challenges associated with this prevalent condition.
Evaluation and Risk Assessment for Dental Implants
In the preparation of osteoporosis patients for dental implant procedures, a meticulous evaluation and risk assessment are crucial components. Dental professionals initiate this process by conducting a comprehensive medical history review to ascertain the patient’s overall health status. This review involves inquiries about the patient’s diagnosis of osteoporosis, duration of the condition, and the use of medications such as bisphosphonates, which are commonly prescribed to manage bone density. Understanding the patient’s pharmaceutical regimen is essential, as certain medications can significantly impact the healing process and integration of the implant.
Additionally, imaging techniques play a vital role in evaluating bone density. Radiographic assessments, including panoramic radiographs or cone-beam computed tomography (CBCT), provide invaluable information regarding the quality and quantity of the bone at the proposed implant site. This imaging helps identify the best placement options and allows for the careful planning of the surgical procedure, ensuring that adequate bone support is available for the implants.
Furthermore, dental professionals must consider additional risk factors that could complicate the implant procedure for patients with osteoporosis. These factors may include age, gender, systemic diseases, and lifestyle choices such as smoking or alcohol consumption, which can all affect bone health and healing. A thorough evaluation of these aspects contributes to the overall risk assessment, facilitating informed decision-making regarding the viability of dental implants for these patients.
By conducting a detailed assessment of the patient’s medical history, understanding medication interactions, evaluating bone density through advanced imaging, and identifying other relevant risk factors, dental professionals can enhance the safety and efficacy of dental implant procedures for individuals managing osteoporosis.
Patient Education and Communication
Effective communication is paramount when preparing osteoporosis patients for dental implant procedures. Given that osteoporosis presents unique challenges in dental health, it is essential that patients are thoroughly educated about the procedure, its potential risks, and alternative treatments available to them. This ensures that patients are not only informed but can make empowered decisions regarding their oral health.
During the initial consultations, dentists should provide comprehensive information about the dental implant procedure. This includes a detailed explanation of how implants are inserted, the materials used, and the expected timeline for recovery. It is also crucial to discuss the implications of osteoporosis on the success of the dental implant. Dentists should explain how the condition affects bone density and, consequently, the integration of the implant into the jawbone.
In addition to the specific procedure details, potential risks associated with dental implants must be communicated. Patients should be aware of possible complications, such as implant failure, infection, and the need for additional surgical procedures. Furthermore, alternative treatment options should be discussed, including dentures or bridgework, allowing patients to weigh the benefits and drawbacks of each approach.
Encouraging open dialogue between the dentist and the patient is essential. Dentists should create an environment where patients feel comfortable voicing their concerns and asking questions. Using open-ended questions can prompt patients to express their thoughts and worries about dental implant procedures. It may also be helpful to provide written resources or educational materials that patients can review at their leisure. This can reinforce the information shared during consultations and empower patients to engage in their treatment process actively.
By prioritizing patient education and fostering effective communication, dental professionals can make a significant positive impact on the treatment experience for osteoporosis patients, improving their outcomes and overall satisfaction.
Collaboration with Medical Professionals
Collaboration with medical professionals is vital when preparing osteoporosis patients for dental implant procedures. Engaging with the patient’s physician or specialist, often an endocrinologist, ensures a comprehensive treatment plan tailored to the individual’s health status and needs. Osteoporosis can significantly affect the quality and durability of the bone, making it essential to assess the patient’s overall medical condition before proceeding with dental implants.
One primary aspect of this collaboration is determining the appropriate timing of the implant procedure. Osteoporosis patients may be on medications that influence bone density and healing, such as bisphosphonates or hormone replacement therapies. Consulting with the prescribing physician can provide critical insights into how these medications may impact surgical outcomes. Adjustments to the patient’s medication regimen may be necessary to optimize bone quality prior to placement of dental implants. For instance, if a patient is on bisphosphonates, the medical team might suggest a temporary pause in the medication, allowing for enhanced bone integration around the implant.
Moreover, dental professionals need detailed medical histories to understand the risks associated with anesthesia and surgery for osteoporosis patients. Certain comorbidities associated with osteoporosis, such as cardiovascular diseases, can complicate surgical procedures. An open line of communication with medical professionals facilitates timely intervention and risk mitigation strategies tailored to the patient’s health profile.
In summary, a unified approach among dental and medical professionals is crucial for ensuring the safety and success of dental implants in osteoporosis patients. By leveraging the expertise of various health practitioners, a comprehensive treatment plan can be designed, addressing all medical considerations for a more effective dental procedure and optimized recovery.
Selecting the Appropriate Dental Implant Technique
When preparing osteoporosis patients for dental implant procedures, the selection of an appropriate dental implant technique is crucial. Osteoporosis can significantly impact the quality and density of the bone, which are vital factors for the success of dental implants. To ensure optimal outcomes, dentists must assess the patient’s bone quality, taking into consideration the severity of the condition and its effect on the jawbone.
One viable option for patients with reduced bone density is the use of mini implants. These smaller implants require less bone mass and, therefore, are more suitable for patients whose jawbone may not support traditional implant sizes. Mini implants can provide enhanced stability and can often be placed with less invasive techniques, making them a favorable choice for individuals suffering from osteoporosis.
In addition to mini implants, the use of grafts is another consideration. Bone grafting procedures can help augment the jawbone, providing a solid foundation for conventional implants. There are various grafting techniques available, including autografts, allografts, and synthetic grafts, each with its unique advantages. The selection of a graft type will depend on the specific circumstances of the patient’s case as well as the surgeon’s expertise.
When determining the most suitable dental implant technique, it is also essential for the dentist to factor in additional considerations such as the patient’s overall health, medications, and lifestyle choices. Each patient’s situation will be unique, thus requiring tailored strategies that can enhance the likelihood of a successful implant procedure. By prioritizing stability and individual assessment, dental professionals can navigate the challenges posed by osteoporosis and improve patient outcomes.
Preparing the Patient for Surgery
Preparing a patient with osteoporosis for dental implant surgery involves multiple considerations to reduce risks and enhance the likelihood of a successful outcome. The first step in this preparation is to undertake a thorough preoperative assessment. This typically includes blood tests to evaluate the patient’s overall health, and radiographic imaging, such as x-rays, to assess the bone structure and density. These diagnostic tools are essential for identifying any potential complications and ensuring that the implant can be adequately supported by the available bone mass.
Dietary recommendations play a crucial role in pre-surgical preparation. Osteoporosis patients are often advised to increase their intake of calcium and vitamin D, both of which are vital for bone health. Foods rich in these nutrients, such as dairy products, leafy greens, and fortified cereals, should be emphasized in the weeks leading up to the surgery. Moreover, hydration must be maintained, as it is important for overall health and recovery.
Medication modifications are another critical aspect of preparation. Patients should review their current medications with their healthcare provider to determine if any adjustments are advisable. Certain medications, such as bisphosphonates or anticoagulants, may need to be paused or altered prior to the surgical procedure to diminish the risk of complications such as delayed healing or excessive bleeding.
Lastly, mental preparation cannot be overlooked. The anxiety associated with surgical procedures can be significant, particularly for those with existing health concerns. Healthcare providers should engage in supportive discussions that address the patient’s fears and provide information on what to expect during the surgery. This approach will ensure that patients feel more at ease and confident, contributing positively to their overall surgical experience.
Post-Operative Care and Monitoring
Post-operative care is crucial for osteoporosis patients undergoing dental implant procedures. Given the unique challenges these patients face, such as reduced bone density and compromised healing abilities, tailored post-operative care can significantly enhance recovery outcomes. One of the primary concerns after the surgery is effective pain management. Patients should be advised on appropriate analgesics and methods to minimize pain, taking into account any underlying medication that may affect healing. It is imperative to develop a personalized pain management plan that suits their specific condition and history.
Infection prevention is another vital aspect of post-operative care, especially for patients with osteoporosis. These individuals may be at a heightened risk for complications due to their condition. Ensuring that the surgical site is kept clean and the use of prophylactic antibiotics may be warranted. Patients should receive education on maintaining oral hygiene, which includes gentle brushing and using antiseptic mouth rinses to reduce the chances of infection.
Moreover, dietary recommendations play a significant role in supporting bone health during recovery. A diet rich in calcium and vitamin D is essential in aiding bone healing and improving implant integration. Patients should be encouraged to consume foods such as dairy products, leafy greens, nuts, and fortified foods. Additionally, proper hydration is essential, as it supports overall health and healing.
Regular follow-ups are imperative for monitoring healing and successful osseointegration of the implant. Dental professionals should schedule these appointments to assess the surgical site and ensure the implant is integrating properly. Understanding the path of recovery allows for timely interventions should any complications arise. Continuous assessment allows for adjustments in care plans, ensuring optimal results for osteoporosis patients during the dental implant recovery process.
Lifestyle Modifications for Better Bone Health
Enhancing bone health is essential for osteoporosis patients, especially during the recovery phase following dental implant procedures. A pivotal factor in achieving optimal bone density and structural integrity is the incorporation of nutritious dietary habits. Nutrition plays a critical role in strengthening bones, and patients should focus on consuming foods rich in calcium and vitamin D. Dairy products, leafy greens, and fortified foods can significantly contribute to improving calcium intake. Additionally, fatty fish such as salmon or mackerel provides necessary vitamin D, which aids in calcium absorption and bone building.
Physical activity is another cornerstone of promoting bone health. Osteoporosis patients should engage in weight-bearing exercises, which can stimulate bone formation and increase overall bone density. Activities such as walking, jogging, and strength training are advantageous in this regard. Low-impact exercises, like yoga or swimming, can also improve balance and flexibility, thereby reducing the risk of falls and fractures. It is essential that patients consult with healthcare professionals before initiating any new exercise programs to ensure that they are suitable for their condition.
Moreover, avoiding harmful behaviors is crucial for maintaining bone health. Smoking negatively impacts bone density and hampers healing processes, making it imperative for patients to refrain from tobacco use. Similarly, excessive alcohol consumption has been linked to increased risk of fractures and impaired bone health. It is advisable for individuals to limit their alcohol intake to moderate levels, as recommended by health authorities. By adopting these lifestyle modifications, osteoporosis patients can significantly enhance their overall recovery and improve long-term bone health.
Conclusion and the Importance of Individualized Care
In conclusion, the management of osteoporosis patients seeking dental implant procedures necessitates a tailored approach that takes into account their unique health profiles and specific needs. Throughout the blog post, we have highlighted several critical factors, including the necessity for comprehensive medical assessments, the evaluation of bone density, and the selection of appropriate implant types and methodologies. Each of these elements plays a vital role in ensuring both the safety and efficacy of the dental procedure.
It is essential for dental professionals to understand the complexities involved in treating patients with osteoporosis. While dental implants can significantly improve the quality of life for these individuals, it requires careful planning and individualized treatment strategies to mitigate risks associated with bone fragility. The collaboration between dentists, physicians, and, when appropriate, orthopedic specialists can enhance the treatment planning process, leading to improved patient outcomes.
Moreover, continuous education and awareness regarding advancements in implant technology and materials can empower dental professionals to innovate their approaches, ensuring they are equipped to manage the unique challenges that osteoporosis may present. Emphasizing communication with patients about their condition and treatment plan fosters trust and encourages adherence to pre- and post-operative instructions, further enhancing the likelihood of success.
Ultimately, personalized care that respects the individual circumstances of each osteoporosis patient is imperative for successful dental implant procedures. By remaining diligent in assessments and treatment plans, dental professionals can navigate the complexities involved and contribute to positive health outcomes for their patients. Ongoing research and clinical guidelines will continue to provide direction for best practices in this field, reaffirming the commitment to high-quality, patient-centered care.
Post Related
Media Resources
Media enquiries
- Office hours:
- Call hours:
- info@all-on-x.online